
Effective policies and strategies to impact this goal include:
Parents are mentally and physically healthy, with particular attention paid to the perinatal period.
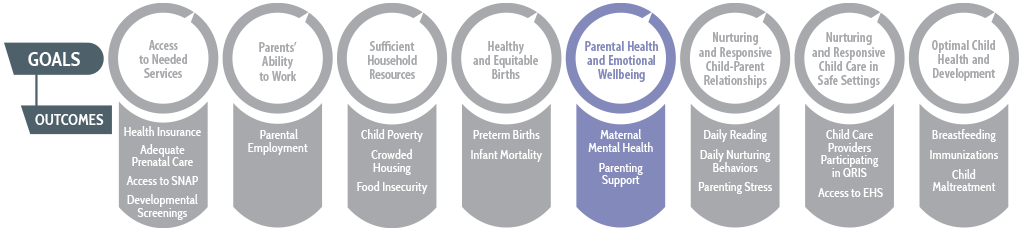
WHY IS PARENTAL HEALTH AND EMOTIONAL WELLBEING AN IMPORTANT PRENATAL-TO-3 GOAL?
Parents’ physical and mental health affects their ability to care for themselves and their children, including their ability to engage in the warm, responsive interactions that infants and toddlers need for long-term healthy development. Yet parents often do not have the resources they need to care for themselves adequately as they care for their children, particularly during the perinatal period, which can pose unique health challenges to families.
Parents without adequate support and resources may experience stress, anxiety, and/or difficulties adjusting to their roles as parents during the prenatal-to-3 period.1 Parental stress has been cited as a risk factor for depression among both mothers and fathers2 and approximately 13% of women with recent live births experienced postpartum depressive symptoms in 2018.3 However, not all mothers get the help they need. A study by the Centers for Disease Control found that among women who had recently given birth, one in eight reported that they had not been asked about depression during postpartum visits, a time when individuals are typically screened and referred to additional services to treat any postpartum concerns.4 Improving parents’ health and emotional wellbeing may boost their ability to respond warmly and sensitively to their infants and toddlers, which will help shape long-term healthy childhood development.5
Due to the social determinants of health—defined by the World Health Organization as “the conditions in which people are born, grow, live, work and age”6—parents who experience substantial adversity are at higher risk of facing physical and mental health challenges.7 These risks perpetuate disparities in children’s health outcomes. For example, due to barriers such as lack of insurance, not all women receive adequate prenatal care, which is critical to ensuring healthy birth outcomes, and women of color are least likely to receive adequate prenatal care.8 The effects of COVID-19 continue to exacerbate these racial and socioeconomic disparities. Data show that COVID-19-related hospitalization rates are approximately 3 times higher for American Indian or Alaska Native, Black, and Hispanic individuals compared to the hospitalization rates for White individuals.8 Other effects of the health crisis, such as stress due to job insecurity and challenges with securing child care, also pose a threat to the mental and physical health of parents who are trying to care for young children.
Because physical and mental health are intertwined, interventions that help relieve parents’ stress also can improve physical health outcomes. Some policies and strategies may impact parental health indirectly by increasing financial resources. Other policies and strategies directly affect parental health by helping parents build social support and reduce stress. In working toward this goal, states can measure progress by tracking outcomes, such as maternal mental health and parenting support, particular to parents with children birth to age 3.
HOW ARE STATES CURRENTLY MEETING THIS PRENATAL-TO-3 GOAL?
Two outcome measures illustrate parents’ health and wellbeing: (1) maternal mental health and (2) parenting support. These outcomes vary considerably across states, and parenting support varies by race and ethnicity as well.
Both outcome measures were calculated intentionally in the negative direction to demonstrate where states have room for improvement and to help states prioritize the prenatal-to-3 policy goals. Out of 51 states, the state lagging furthest behind ranks 51st, and the leading state ranks first. The median state indicates that half of states have outcomes that measure better than that state, whereas half of states have outcomes that are worse. Importantly, the “leading” state on a given outcome does not necessarily indicate a target for all other states to strive toward; even in the states with the best outcomes, many children and families are struggling.
OUTCOME MEASURE: POOR MATERNAL MENTAL HEALTH
% children under age 3 whose mother reports fair/poor mental health
Median state value: 5.0%
Maternal mental health is a strong predictor of healthy child development. In the five lagging states, approximately 9% to 13% of children under age 3 have a mother who has mental health concerns, compared to 2% to 3% of children in the five leading states. Although rates of maternal mental health vary substantially across states, rates do not vary as substantially by race and ethnicity.
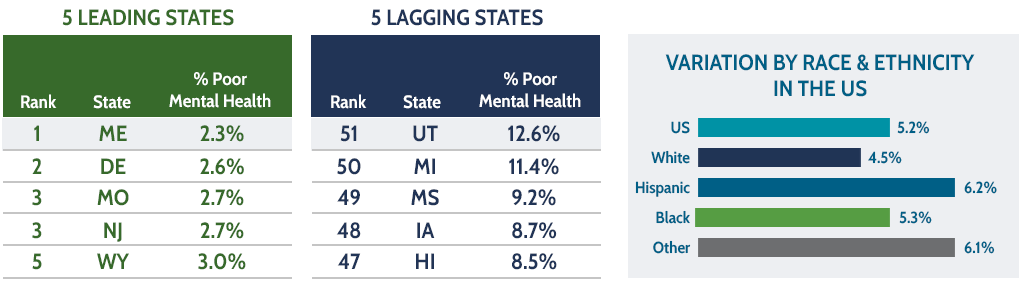
Source: 2018-2020 National Survey of Children’s Health (NSCH).
OUTCOME MEASURE: LOW PARENTING SUPPORT
% children under age 3 whose parent lacks parenting support
Median state value: 14.8%
In the five lagging states, more than one-fifth of children under age 3 have a parent who reports that they do not have anyone they can turn to for emotional support with parenting, compared to less than 8% in the five leading states. Rates of low parenting support vary substantially by race and ethnicity, with approximately 27% of Hispanic children, 19% of Black children, and 9% of White children under age 3 living with a parent who lacks emotional support.
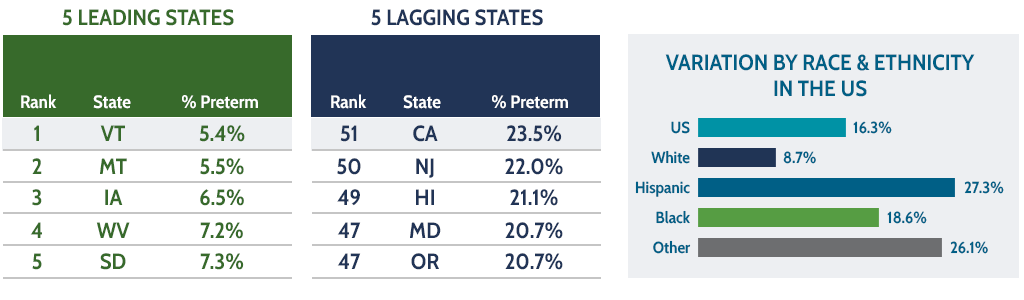
Source: 2018-2020 National Survey of Children’s Health (NSCH).
For additional information regarding calculation details, data quality, and source data please refer to Methods and Sources.
For more information on outcomes by goal, including by race and ethnicity and state, see the 2022 Prenatal-to-3 State Policy Roadmap section on outcomes across the US.
WHAT ARE THE MOST EFFECTIVE POLICIES AND STRATEGIES TO IMPACT PARENTAL HEALTH AND EMOTIONAL WELLBEING?
Based on comprehensive reviews of the most rigorous evidence available, the Prenatal-to-3 Policy Impact Center identified 11 effective solutions that foster the nurturing environments infants and toddlers need. For each of the five policies, the evidence points to a specific policy lever that states can implement to impact outcomes. For the six strategies, the evidence clearly links the strategy to PN-3 outcomes, but the current evidence base does not provide clear guidance on how states should implement each strategy to positively impact outcomes. Four policies and strategies have demonstrated effectiveness at improving parental health and emotional wellbeing.
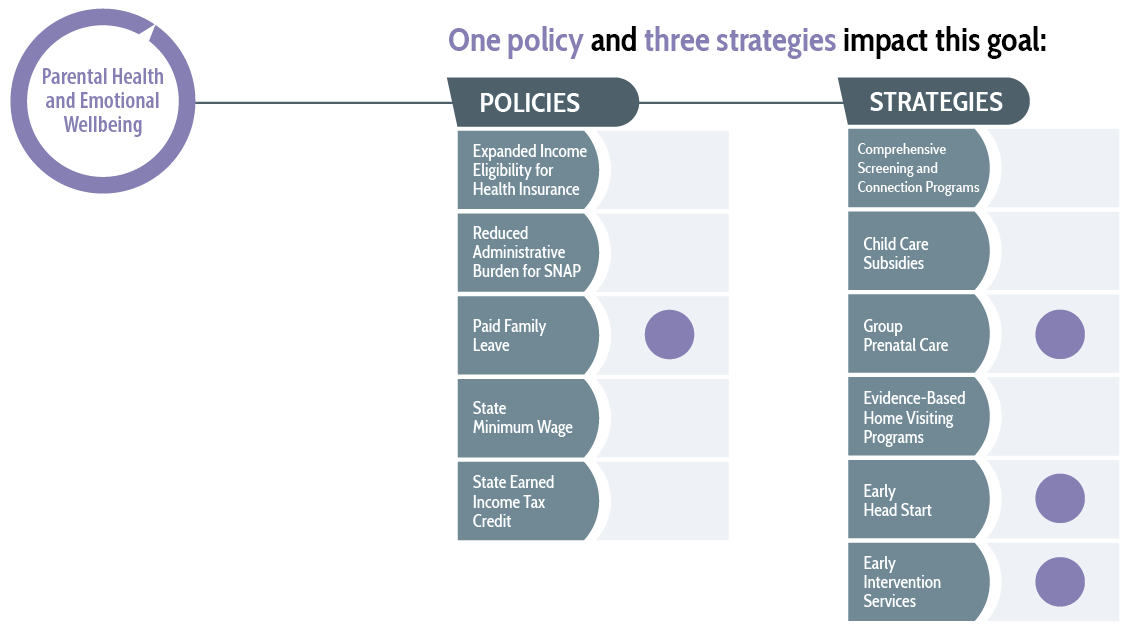
For more information on the impact of state-level policies and strategies in the prenatal-to-3 period, search the Prenatal-to-3 Policy Clearinghouse for an ongoing inventory of rigorous evidence reviews. To learn more about the impact of effective policies and strategies on the eight prenatal-to-3 policy goals, see the Prenatal-to-3 State Policy Roadmap.
WHAT OTHER SOLUTIONS ARE STATES PURSUING THAT CAN HELP BUILD THE EVIDENCE BASE?
Beyond the policies and strategies proven effective by the current research, states also are pursuing other approaches that hold promise for improving parental health and emotional wellbeing; these approaches have not yet accumulated enough rigorous research to enable drawing conclusions on their effectiveness, or the Prenatal-to-3 Policy Impact Center has not yet conducted a comprehensive evidence review for the approach. Other solutions states are pursuing that can help build the evidence base on parental health and emotional wellbeing include, but are not limited to:
- Perinatal mental health programs, which include a variety of efforts at the state and local levels to address parents’ and families’ mental health needs during and after pregnancy (e.g., providing direct mental health resources to families or improving healthcare providers’ capacity to serve pregnant and postpartum women and their children);9
- Targeted screenings, which assess a patient’s specific health risks before problems develop (e.g., postpartum depression and anxiety screenings);10
- Paid sick leave policies, which allow employees to earn paid time off for short-term medical needs; and
- Perinatal telehealth services, including the use of technology to support the provision of health care.
SOURCES
- Rolle, L. et al. (2017). Parenting stress, mental health, dyadic adjustment: A structural equation model. Frontiers in Psychology, 8, 839. doi: 10.3389/fpsyg.2017.00839
- Vismara et al. (2016). Perinatal parenting stress, anxiety, and depression outcomes in first-time mothers and fathers: A 3- to 6-months postpartum follow-up study. Frontiers in Psychology, 7, 938. doi:10.3389/fpsyg.2016.00938
- Bauman, B. L., Ko, J. Y., Cox, S., D’Angelo, D. V., Warner, L., Folger, S., Tevendale, H. D., Coy, K., C., Harrison, L., Barfield, W. D. (2020, May 15). Vital signs: Postpartum depressive symptoms and provider discussions about perinatal depression-United States, 2018. Morbidity and Mortality Weekly Report, 69, 575–581. http://dx.doi.org/10.15585/mmwr.mm6919a2
- Bauman, B. L., Ko, J. Y., Cox, S., D’Angelo, D. V., Warner, L., Folger, S., Tevendale, H. D., Coy, K., C., Harrison, L., Barfield, W. D. (2020, May 15). Vital signs: Postpartum depressive symptoms and provider discussions about perinatal depression-United States, 2018. Morbidity and Mortality Weekly Report, 69, 575–581. http://dx.doi.org/10.15585/mmwr.mm6919a2
- Center on the Developing Child. Serve and return. Harvard University. https://developingchild.harvard.edu/science/key-concepts/serve-and-return/
- World Health Organization. (n.d.). Social determinants of health. https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1
- Braveman, P., & Gottlieb, L. (2014). The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports, 129(Suppl 2): 19-31. https://doi:10.1177/00333549141291S206
- Novoa, C. (2020, January 31). Ensuring healthy births through prenatal support: Innovations from three models. Center for American Progress. https://www.americanprogress.org/issues/early-childhood/reports/2020/01/31/479930/ensuring-healthy-births-prenatal-support
- Maternal Health Task Force. (n.d.). Perinatal mental health. Harvard Chan School Center of Excellence in Maternal and Child Health. https://www.mhtf.org/topics/perinatal-mental-health/
- Office of Disease Prevention and Health Promotion. (n.d.). Get screened. HHS. https://health.gov/myhealthfinder/topics/doctor-visits/screening-tests/get-screened#text=Screenings%20are%20medical%20tests%20that,can%20do%20for%20your%20health.
