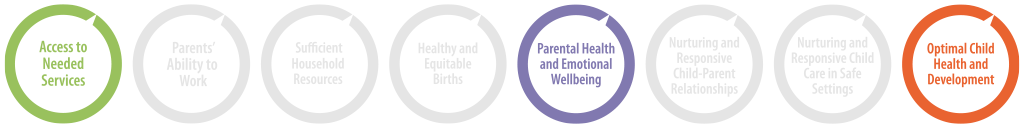
Group Prenatal Care positively impacts these strategy goals:
SUMMARY
Group prenatal care is an effective state strategy to impact:
Participation in group prenatal care increases the likelihood that mothers receive adequate prenatal care, improve mothers’ physical and mental health, and increases breastfeeding initiation. Rigorous evaluations on group prenatal care have demonstrated an improvement in adequate prenatal care and development outcomes. Although group prenatal care has not been studied as a statewide intervention more evidence is needed to provide states with guidance on the most effective way to implement group prenatal care models that promote healthy, equitable births statewide.
Prenatal care generally refers to individual patient care received from one obstetric care provider during an individual’s pregnancy. Group prenatal care (GPNC) is an alternative model of care facilitated by a trained health care provider and delivered in a group setting; integrating health assessments, education, skill building, and peer support. GPNC provides pregnant people (typically with low-risk pregnancies not requiring individual monitoring) with more hours of care compared to traditional individual care.
States vary in how they financially support group prenatal care. They can offer an enhanced Medicaid reimbursement rate for GPNC, provide grant funding to communities or providers to offer the model, or implement Alternative Payment Models that incentivize enhanced maternity care. The current evidence base does not provide clear guidance on how states can best support and implement group prenatal care for pregnant people who prefer the group approach.
Download the Complete Evidence Review
Group Prenatal Care Evidence Review (PDF)
Download the 2-Page Summary
Summary of the Rigorous Research on Group Prenatal Care (PDF)
Recommended Citation:
Prenatal-to-3 Policy Impact Center. (2023). Prenatal-to-3 policy clearinghouse evidence review: Group prenatal care (ER 08D.0923). Peabody College of Education and Human Development, Vanderbilt University. https://pn3policy.org/policy-clearinghouse/group-prenatal-care
Updated September 2023



